WHAT IS PERI-IMPLANT DISEASE?
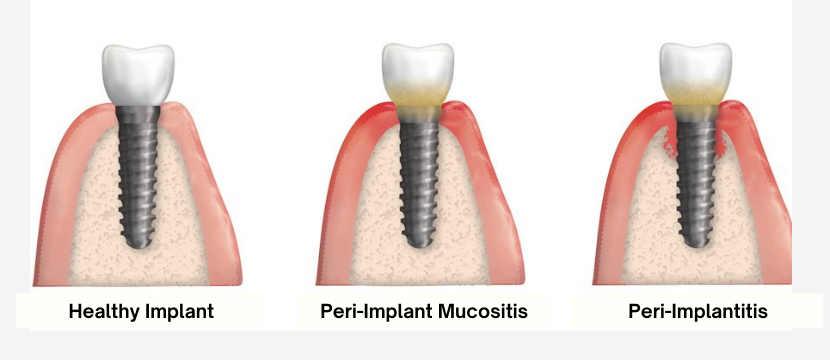
Peri-implant diseases are inflammatory conditions affecting the soft tissue (gum) and hard tissue (bone) around dental implants.
PERI-IMPLANT DISEASE IS CLASSIFIED INTO TWO CATEGORIES – PERI-IMPLANT MUCOSITIS AND PERI-IMPLANTITIS.
In peri-implant mucositis, gum inflammation is found only around the soft tissues of the dental implant, with no signs of bone loss. Generally, peri-implant mucositis is a precursor to peri-implantitis. Evidence suggests that peri-implant mucositis may be successfully treated and is reversible if caught early.
In peri-implantitis, gum inflammation is found around the soft tissue and there is deterioration in the bone supporting the dental implant. Peri-implantitis usually requires surgical treatment.
WHAT CAUSES PERI-IMPLANT DISEASE?
Just like with a natural tooth, bacteria can build up below the gum line at the base of the implant. Over time, the bacteria irritate the soft tissue, causing inflammation and damage (peri-implant mucositis). If left untreated, the disease will progress and cause hard tissue damage - deterioration of the bone structure below the implant (peri-implantitis).
Because an implant cannot attach as easily to the gums as natural teeth, the gum tissue around an implant if often looser than the gum tissue around a natural tooth which leaves extra space for bacteria to grow. This means that the risk of inflammation is much higher. Of all implant patients, more than 40% are affected by inflammation around the implant.
SIGNS AND SYMPTOMS OF PERI-IMPLANT DISEASE:
If you have implants and have one or more of the following symptoms, you should contact your dentist or hygienist as soon as possible.
- Inflammation of the gums
- Bleeding gums
- Redness and swelling in the gum tissue around the implant
- Receding gums
- Pocket formation between the gums and the dental implant
- Visible dental implant threads
- Loosened dental implant
- Pus in the gums around the dental implant
- Unpleasant taste in the mouth
- Jaw pain due to bone deterioration
HOW CAN PERI-IMPLANT DISEASE BE PREVENTED?
Taking proper care of your dental implants and committing to a daily cleaning routine like the one below can prevent peri-implant disease.
- Brush at least twice a day, using a soft-bristled toothbrush. Soft bristles are less likely to damage your gums or cause bleeding and are just as effective as medium or hard bristles at removing tartar and plaque. Electric toothbrushes are shown to disrupt and remove bacteria from teeth more effectively than manual toothbrushes due to the way they generate a higher number of brush strokes than the human hand. Whether you choose an electric or manual toothbrush, make sure it has soft bristles. Brushing in the morning after you wake up eliminates morning breath and removes bacteria that has built up in the mouth overnight. Brushing in the evening before bedtime helps remove bacteria that has built up throughout the day and reduces the risk for plaque buildup and decay overnight. Many dentists encourage brushing after every meal, or anytime during the day as needed to remove food debris and bacteria.
- Use an oral irrigator. An oral irrigator disrupts and removes bacteria in pocket depths up to 6 mm deep. Many oral irrigators come with rubber-tip stimulators and other attachments designed to accommodate sensitive gums and effectively clean hard-to-reach areas between teeth. Many dentists recommend oral irrigators over dental floss, since some brands of floss can shed particles that contribute to peri-implant disease. Be sure to use the oral irrigator first to prevent washing away the fluoride introduced from brushing and flossing.
- Use crown and bridge floss. Crown and bridge floss is specially designed to scrub under and around dental implants. It has two stiff nylon ends and a fuzzy middle which gently cleans the dental implant surface and the porcelain that touches the gum line. The stiff ends enable you to insert the floss between the dental implants at the gum line and pull it through to the other side. You can then lean it against the implant surface and rub it side to side. It’s a good idea to use this floss after brushing while the toothpaste residue is still in your mouth. This enables you to distribute the fluoride around the implant, which helps prevent unwanted bacterial growth.
- Use low-abrasive toothpaste. Use toothpaste that lacks abrasive ingredients such as baking soda or stain-remover agents, since these ingredients may wear on acrylic and remove glaze from porcelain implants. Look for toothpaste specifically made for use on dental implants or ask your dentist for toothpaste recommendations.
- Brush under and around the dental implant crown. Bacteria and plaque may accumulate under and around the implant crown to increase the risk for peri-implant disease. To reach these areas, try using an angled-neck toothbrush or an interdental brush with a slim head—especially if your implant is located at the back of your mouth.