Gum Disease
What causes gum disease?
Our mouths are full of bacteria. These bacteria, along with mucus and other particles, constantly form a sticky, colorless plaque on teeth. Brushing, flossing and using the Hydro Floss® help get rid of plaque. Plaque that is not removed can harden and form calculus (also known as tartar) that brushing can't remove. Only a professional cleaning by a dentist or dental hygienist can remove calculus.
Gingivitis
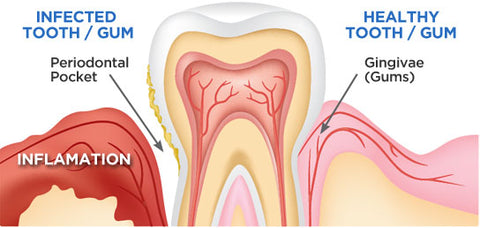
The longer plaque and calculus are on teeth, the more harmful they become. The bacteria cause inflammation of the gums that is called gingivitis. With gingivitis, the gums become red, swollen and can bleed easily. Gingivitis is a mild form of gum disease that can usually be reversed with daily brushing, flossing, use of the Hydro Floss® and regular cleaning by a dentist or dental hygienist. This form of gum disease does not include any loss of bone and tissue that hold teeth in place.
Periodontitis
When gingivitis is not treated, it can advance to periodontitis (which means inflammation around the tooth). In periodontitis, gums pull away from the teeth and form spaces, called pockets, that become infected. The body’s immune system fights the bacteria as the plaque spreads and grows below the gum line. Bacterial toxins and the body’s natural response to infection start to break down the bone and connective tissue that hold teeth in place. If not treated, the bones, gums, and tissue that support the teeth are destroyed. The teeth may eventually become loose and have to be removed.
Progression of gum disease:

Risk Factors
- Need another reason to quit smoking? Smoking is one of the most significant risk factors associated with the development of gum disease. Additionally, smoking can lower the chances for successful treatment.
- Hormonal changes in girls/women. These changes can make gums more sensitive and make it easier for gingivitis to develop.
- People with diabetes are at higher risk for developing infections, including gum disease.
- Auto immune diseases and their treatments can also negatively affect the health of gums, as can treatment for cancer.
- There are hundreds of prescription and over the counter medications that can reduce the flow of saliva, which has a protective effect on the mouth. Without enough saliva, the mouth is vulnerable to infections such as gum disease. And some medicines can cause abnormal overgrowth of the gum tissue; this can make it difficult to keep teeth and gums clean.
- Genetic susceptibility. Some people are more prone to severe gum disease than others.
Who gets gum disease?
People usually don’t show signs of gum disease until they are in their 30's or 40's. Men are more likely to have gum disease than women. Although teenagers rarely develop periodontitis, they can develop gingivitis, the milder form of gum disease. Most commonly, gum disease develops when plaque is allowed to build up along and under the gum line and harden into calculus.
Symptoms of gum disease include:
- Bad breath that won’t go away
- Red or swollen gums
- Tender or bleeding gums
- Painful chewing
- Loose teeth
- Sensitive teeth
- Receding gums or teeth that appear longer than normal
Any of these symptoms may be a sign of a serious problem and should be checked by a dentist. At your dental visit the dentist or hygienist should:
- Ask about your medical history to identify underlying conditions or risk factors (such as smoking) that may contribute to gum disease.
- Examine your gums and note any signs of inflammation.
- Use a tiny ruler called a probe to check for and measure any pockets. In a healthy mouth, the depth of these pockets is usually between 1 and 3 millimeters. The test for pocket depth is usually painless.